Trauma Disorders
Posttraumatic Stress Disorder (PTSD)
KEY FEATURES. Following exposure to a traumatic event, the individual develops a characteristic cluster of symptoms across four categories (intrusion, avoidance, negative changes in thoughts and/or mood, and reactivity). While posttraumatic symptoms often resolve through a natural recovery process, at times that process is interrupted or stalled and PTSD develops. The diagnosis of PTSD is made if the symptoms have been present for more than 1 month after the traumatic event. If the symptoms have lasted for less than 1 month, the diagnosis of Acute Stress Disorder may be made.
REMEMBER: Having PTSD does not make one weak or defective or otherwise at fault. Although the symptoms are frightening and can be severe, this is a highly treatable disorder.
PREVALENCE. The 12-month prevalence in the general population is approximately 3.5%. However, certain individuals are significantly more likely to experience PTSD. These include military personnel, first responders, and survivors of rape. Women are more likely to develop PTSD and experience it for a longer duration. Some of the increased risk appears to be due to a greater likelihood of exposure to interpersonal violence.
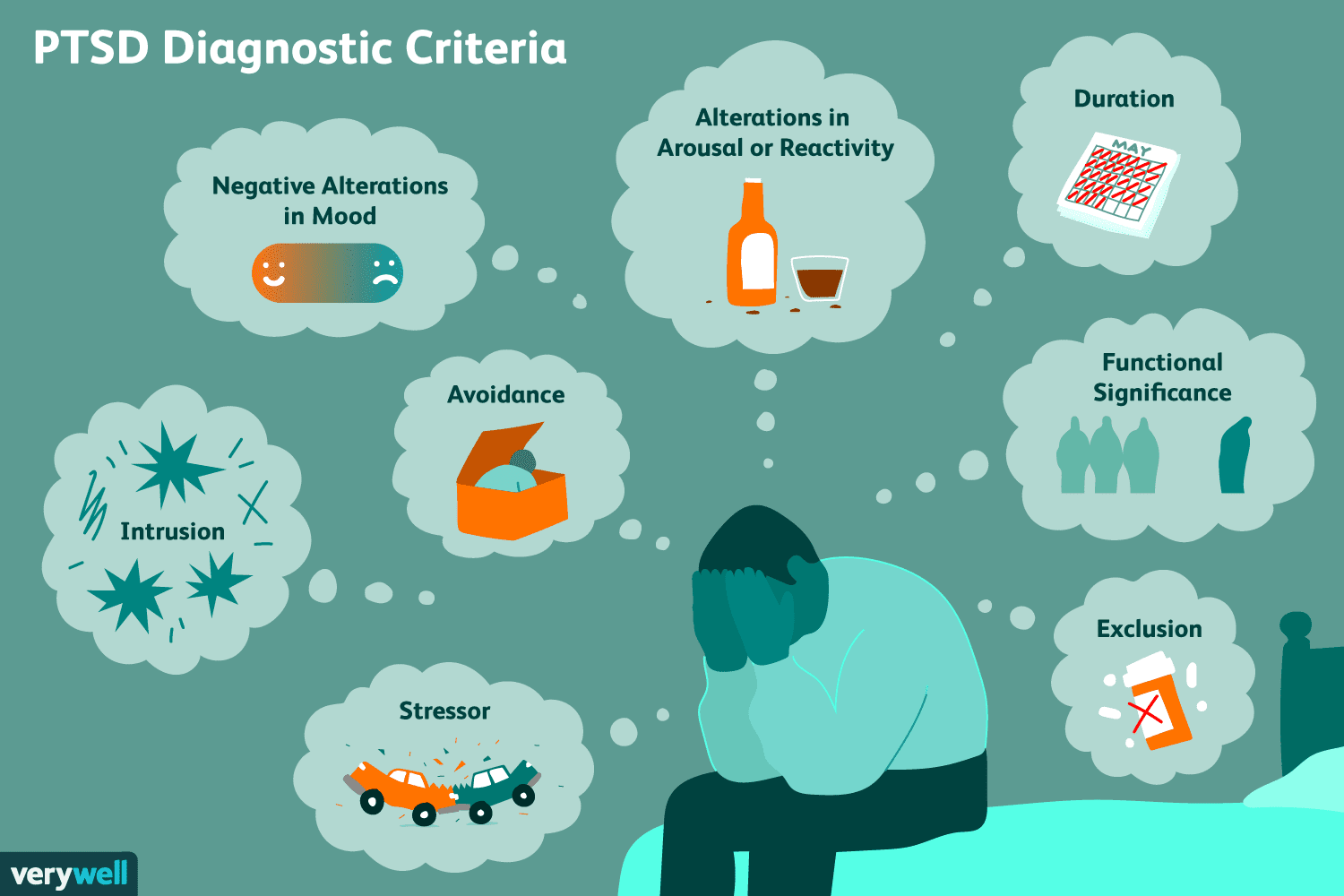
DIAGNOSTIC CRITERIA. The diagnostic criteria for this disorder include a combination of (1) exposure to specific types of traumatic events and (2) subsequent symptoms grouped into four categories.
The Traumatic Event
You have been exposed to a traumatic event that was actual or threatened death, sexual violence, or serious injury, in one or more of the following ways:
- Directly experiencing the event (it happened to you)
- Directly experiencing repeated or extreme exposure to the details of the event (e.g., first responders collecting human remains, police officers repeatedly exposed to details of child abuse)
- Witnessing the event in person as it occurred to others
- Learning that the event occurred to a close family member or close friend (in this case, actual or threatened death must have been violent or accidental)
The Four Categories of Symptoms
The four categories are intrusion, avoidance, negative thoughts and/or mood, and reactivity, beginning after the event occurred. Although there is a total of 20 symptoms across these categories, it is not necessary to have all of them in order to meet the clinical threshold.
Intrusion Symptoms
- Recurrent, involuntary, and intrusive distressing memories of the traumatic event
- Recurrent distressing dreams in which the content and/or emotion of the dream are related to the event
- Dissociative reactions (e.g., flashbacks), in which you feel or act as if the event were recurring
- Intense or prolonged psychological distress in response to internal or external triggers that resemble or symbolize an aspect of the event
- Marked physiological reactions in response to internal or external triggers that resemble or symbolize an aspect of the event
Avoidance Symptoms
- Avoidance or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the event
- Avoidance or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the event
Negative Alterations in Cognition and/or Mood
- Inability to remember an important aspect of the event, typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs
- Persistent and exaggerated negative beliefs or expectations about yourself, others, or the world (e.g., “I’m bad,” “No one can be trusted,” “The world is completely dangerous,” “My whole nervous system is permanently ruined”)
- Persistent, distorted thoughts about the cause or consequences of the event that lead you to blame yourself or others
- Persistent negative emotions, such as fear, horror, anger, guilt, or shame
- Markedly diminished interest or participation in significant activities
- Feelings of detachment or estrangement from others
- Persistent inability to experience positive emotions (e.g., happiness, satisfaction, or loving feelings)
Alterations in Arousal and Reactivity
- Irritable behavior and angry outbursts (quick tempered, with little or no provocation), typically expressed as verbal and/or physical aggression (e.g., yelling at people, getting into fights, destroying objects)
- Reckless or self-destructive behavior, such as dangerous driving, excessive alcohol or drug use, or self-injurious or suicidal behavior
- Hypervigilance, which means heightened sensitivity to potential threats, whether related to the traumatic event (e.g., because you were in a car accident, you are extra sensitive to the dangers of traffic) or completely unrelated (e.g., you were in a car accident, but you keep worrying that you are going to suffer a heart attack)
- Exaggerated startle response, which causes heightened sensitivity to unexpected sudden stimuli such as loud noises or movements (in general, it is an involuntary, reflexive mental and physical reaction, with examples such as flinching, jumping, gasping, flexion of muscles, trembling, palpitation, dry mouth, and a feeling of instant fear or panic)
- Problems with concentration, such as difficulty remembering daily events or attending to focused tasks
- Difficulty falling or staying asleep, which may be associated with nightmares and safety concerns or with generalized elevated arousal that has been interfering with sleep
Additional Diagnostic Criteria
- You have been experiencing the above symptoms for more than 1 month after having been exposed to the traumatic event
- The symptoms cause you significant distress or impairment in social, occupational, or other important areas of functioning
ASSOCIATED FEATURES. In addition to the diagnostic criteria, an individual with PTSD may also experience auditory pseudo-hallucinations (e.g., hearing your thoughts spoken in one or more different voices), paranoid ideation, or dissociative symptoms, as well as difficulties in regulating emotions or maintaining stable relationships.
DEVELOPMENT & COURSE. Symptoms typically begin within the first 3 months after the traumatic event (although the diagnosis is not made until after the first month). For some, there may be a delay of months, or even years, before the symptoms reach the clinical threshold. It is also possible for some individuals to have a delayed expression of symptoms, in which some of the symptoms appear immediately but there are not enough of them to meet the full diagnostic criteria. Different symptoms may have different duration and intensity. While some individuals reach full recovery within 3 months (about 50% of adults do), others may remain symptomatic for more than a year, for multiple years, or at times even for decades.
Acute Stress Disorder (ASD)
KEY FEATURES. Following exposure to a traumatic event, the individual develops a characteristic cluster of symptoms across five categories (intrusion, negative mood, dissociation, avoidance, and reactivity) lasting from 3 days to 1 month (after 1 month, the diagnosis of PTSD may be made).
As you read the diagnostic criteria below, you will see that they very much resemble those for PTSD.
PREVALENCE. The prevalence rates differ based on the nature of the traumatic event and the context in which it is assessed. In cases of motor vehicle accidents, 13%-21% will develop the disorder; 14% in mild traumatic brain injuries; 10% in severe burns; and 6%-12% in cases of industrial accidents. When the event is interpersonal violence, such as assault, rape, or witnessing a mass shooting, the prevalence is 20%-50%. As with PTSD, women are more likely to develop the disorder. Some of the increased risk appears to be due to a greater likelihood of exposure to interpersonal violence (including sexual assault), as well as to possible neurobiological differences in stress response.
DIAGNOSTIC CRITERIA. The diagnostic criteria for this disorder include a combination of (1) exposure to specific types of traumatic events and (2) subsequent symptoms grouped into five categories.
The Traumatic Event
You have been exposed to a traumatic event that was actual or threatened death, sexual violence, or serious injury, in one or more of the following ways:
- Directly experiencing the event (it happened to you)
- Directly experiencing repeated or extreme exposure to the details of the event (e.g., first responders collecting human remains, police officers repeatedly exposed to details of child abuse)
- Witnessing the event in person as it occurred to others
- Learning that the event occurred to a close family member or close friend (in this case, actual or threatened death must have been violent or accidental)
The Five Categories of Symptoms
You have been experiencing symptoms from any of the five categories of intrusion, negative mood, dissociation, avoidance, and reactivity, beginning or worsening after the event occurred. Although there is a total of 14 symptoms across these categories, it is not necessary to have all of them in order to meet the clinical threshold.
Intrusion Symptoms
- Recurrent, involuntary, and intrusive distressing memories of the traumatic event
- Recurrent distressing dreams in which the content and/or emotion of the dream are related to the event
- Dissociative reactions (e.g., flashbacks), in which you feel or act as if the event were recurring
- Intense or prolonged psychological distress or marked physiological reactions in response to internal or external triggers that resemble or symbolize an aspect of the event
Negative Mood
- Persistent inability to experience positive emotions (e.g., happiness, satisfaction, or loving feelings)
Dissociative Symptoms
- An altered sense of the reality of your surroundings or yourself (e.g., seeing yourself from someone else’s perspective, being in a daze, time slowing)
- Inability to remember an important aspect of the event, typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs
Avoidance Symptoms
- Efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the event
- Efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the event
Reactivity Symptoms
- Irritable behavior and angry outbursts (quick tempered, with little or no provocation), typically expressed as verbal and/or physical aggression (e.g., yelling at people, getting into fights, destroying objects)
- Hypervigilance, which means heightened sensitivity to potential threats, whether related to the traumatic event (e.g., because you were in a car accident, you are extra sensitive to the dangers of traffic) or completely unrelated (e.g., you were in a car accident, but you keep worrying that you are going to suffer a heart attack)
- Exaggerated startle response, which causes heightened sensitivity to unexpected sudden stimuli such as loud noises or movements (in general, it is an involuntary, reflexive mental and physical reaction, with examples such as flinching, jumping, gasping, flexion of muscles, trembling, palpitation, dry mouth, and a feeling of instant fear or panic)
- Problems with concentration, such as difficulty remembering daily events or attending to focused tasks
- Difficulty falling or staying asleep, which may be associated with nightmares and safety concerns or with generalized elevated arousal that has been interfering with sleep
Additional Diagnostic Criteria
- You have been experiencing the above symptoms for 3 days to 1 month after having been exposed to the traumatic event
- The symptoms cause you significant distress or impairment in social, occupational, or other important areas of functioning
ASSOCIATED FEATURES. In addition to the diagnostic criteria, individuals with ASD may experience symptoms that are not required for the diagnosis. For example, they may have extremely negative thoughts about their role in the traumatic event or their response to it (e.g., guilt for not preventing it or for not coping better). In addition, panic attacks are common in the first month after the event. They may be triggered by reminders or occur spontaneously. Individuals may also engage in chaotic or impulsive behavior, such as driving recklessly, making irrational decisions, or gambling. It is also not uncommon to experience “postconcussive symptoms” (regardless of whether there has been an actual mild traumatic brain injury) such as headaches, dizziness, sensitivity to light or sound, irritability, and concentration deficits.
DEVELOPMENT & COURSE. The diagnosis is not made until 3 days after the traumatic event has occurred. If the symptoms persist beyond 1 month, the diagnosis of PTSD may be made. Approximately 50% of individuals who eventually develop PTSD initially meet the criteria for ASD. It is possible for the symptoms to worsen during the first month, whether as a result of ongoing life stressors or additional traumatic events.
RISK FACTORS. Risk factors include prior mental disorder(s), neuroticism (one of the personality traits included in the Five-Factor Model), perception of greater severity of the traumatic event, and an avoidant coping style. A particularly strong risk factor is the tendency to “catastrophize,” which causes the individual to have an exaggerated perception of future harm, guilt, or hopelessness.
Adjustment Disorders
There are six distinct adjustment disorders, each with its own diagnostic code.
KEY FEATURES. The presence of emotional and/or behavioral symptoms in response to an identifiable stressor occurring within 3 months of the onset of the stressor.
Most people have stress reactions when something negative happens to them. This is not necessarily an adjustment disorder. The diagnosis is only made when the magnitude of the distress exceeds what would normally be expected or when the stressful event causes significant impairment in functioning.
Important: While the symptoms of an adjustment disorder may not appear as severe as those of PTSD and ASD, individuals with adjustment disorders are at an increased risk of suicide attempts and completed suicide.
STRESSORS. There may be just one stressor (e.g., divorce, termination of a romantic relationship, involuntary job termination, change of jobs) or multiple simultaneous stressors (e.g., work difficulties and marital problems). Stressors may be recurrent (e.g., a seasonal business crisis) or continuous (e.g., living in a crime-ridden neighborhood, having a chronic illness with increasing disability). Some stressors are associated with specific phase of life events, such as beginning school, leaving or returning to parental home, getting married, becoming a new parent, or retiring. Lastly, the stressor may be something that affects just one individual, an entire family, or a larger group or community (e.g., as in a natural disaster).
PREVALENCE. Adjustment disorders are common, but their prevalence varies widely. For individuals in outpatient mental health treatment, the prevalence is approximately 5%-20%; for those in a hospital psychiatric consultation setting, it frequently reaches 50%.
DIAGNOSTIC CRITERIA. You may be suffering from an adjustment disorder if you have developed the following symptoms within 3 months after the onset of an identifiable stressor:
- Significant distress that is out of proportion to the severity or intensity of the stressor, taking into account the external context and the cultural factors that might influence symptom severity
- The symptoms have caused you significant impairment in social, occupational, or other important areas of functioning
- Once the stressor or its consequences have terminated, the symptoms do not persist for more than an additional 6 months
- With depressed mood: If most of your symptoms are low mood, tearfulness, or feelings of hopelessness
- With anxiety: If most of your symptoms are nervousness, worry, or jitteriness
- With mixed anxiety and depressed mood: If most of your symptoms are a combination of #3 and #4
- With disturbance of conduct: If most of your symptoms involve behaviors such as excessive anger, rage, or substance abuse, or behaviors that violate the rights of others or fall outside of major age-appropriate societal norms and rules (e.g., truancy, vandalism, reckless driving, fighting, defaulting on legal responsibilities)
- With mixed disturbance of emotions and conduct: If most of your symptoms are a combination of depressed mood (#4) and/or anxiety (#5) and disturbance of conduct (#7)
- Unspecified: If most of your symptoms do not fall into one of the above categories (e.g., physical complaints, social withdrawal, or work or school performance issues)
DURATION. As indicated above, the symptoms are supposed to start within 3 months of the onset of the stressor and cannot persist for more than 6 months after the termination of the stressor or its consequences. However, it is recognized that there are chronic stressors or those that have enduring consequences. Therefore, the DSM-5 provides two specifiers that address duration: Acute for when the symptoms last 6 months or less, and Persistent (chronic) for when the symptoms last 6 months or longer.
How is an adjustment disorder different from bereavement? You may be diagnosed with an adjustment disorder following the death of a loved one when the intensity or persistence of grief reactions exceeds what normally might be expected. Conversely, bereavement is defined as an expected response to the loss, with symptoms such as intense yearning for the deceased, intense sorrow and emotional pain, preoccupation with thoughts and memories of the deceased, feelings of emptiness and loss, at times thoughts of having failed the deceased (e.g., “I should have visited him more while he was still alive,” “I didn’t tell her enough how much I loved her”), or even thoughts of wanting to “join” the deceased (but not actually following through).
Another point to make is that in the DSM-5, bereavement is not classified as a mental disorder. Instead, it is included in the back of the manual under “Other Conditions” and assigned a “Z” code.
Content based in part on the following two public domain sources:
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013
- National Institute of Mental Health publications
